With such an enormous impact now and into the future, we can’t afford to ignore dementia
Mark MacDonald, Associate Director of Evidence, Policy and Influencing
| Alzheimer’s Society
Many of you reading this will already know the impact of dementia on those living with it. It’s a profound personal and family challenge, but the impact doesn’t end behind closed doors. The pressure on the NHS, social care, and the huge personal and economic costs present the most urgent health challenge of our time.
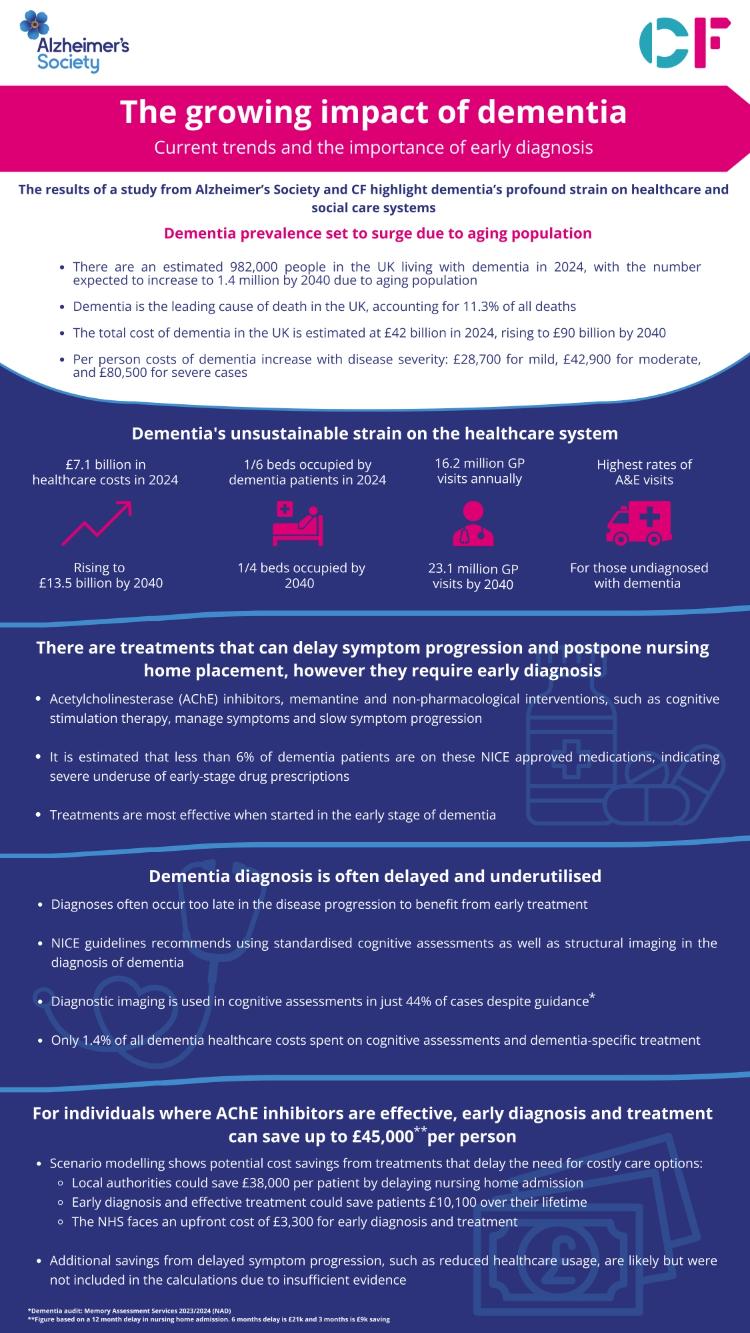
The numbers are daunting. £42bn a year now, rising to £90bn in just 15 years. Tragically, that cost of falls most heavily on those living with the condition and their carers (63%) whilst it is estimated dementia will cost social care £17.2bn and the healthcare system £7.1bn this year alone*.
With prevalence rates expected to grow from around 1million in the UK today to 1.4million by 2040 the cost of dementia is set to balloon to £90bn by 2040. New evidence Alzheimer’s Society is bringing to the table is shining a light on the scale and urgency of the challenge but – for the first time – clear, evidence-based actions to ease pressure and reduce cost.
Policymakers’ range of responses to dementia had been thought to be limited. The status quo of relentlessly building pressure and cost is not inevitable. There are clear, positive choices that can and must be made to support the NHS, social care and individuals address the challenge presented by dementia now and into the future. Prioritising dementia now is critical.
Diagnosis is a sound investment
Despite the hefty price tag of failing to address the challenges of dementia, spending on diagnosis and treatment is equivalent to just 1.4% of dementia healthcare costs.
The UK’s aim is that two-thirds of people with dementia will get a diagnosis and we’re not even reaching that target, which a Labour Health Minister has already acknowledged as not ambitious enough. Diagnosing someone with the UK’s biggest killer is more than just a moral duty. It unlocks certainty and access to support which directly translates into reduced system pressure.
Research highlights the importance of timely and accurate diagnosis, yet diagnostic imaging accounts for less than 0.1% of the total healthcare cost of dementia. NICE guidance states that if the diagnosis is uncertain, patients should receive imaging tests. It is estimated only 3.8% of people with suspected dementia received an imaging test per year.
The lack of ambition on dementia diagnosis is a huge missed opportunity.
In dementia, the earlier the diagnosis, the bigger the potential cost saving - and the better for the individuals affected.
Acting early has a huge impact
Alzheimer’s Society research commissioned from Carnall Farrar on the economic impact of dementia found that the average annual cost of dementia per person increases as the condition progresses at £28,700 for mild dementia, £42,700 for moderate dementia and £80,500 for severe dementia. These are enormous cost differences which suggest that intervening early and effectively is critical.
By diagnosing people just one year earlier and providing access to these NICE-approved treatments where they are effective**, the modelling suggests there could be savings of tens of thousands of pounds by delaying the onset of severe symptoms.
By delaying the impact of severe symptoms, people with dementia can enjoy their independence and a better quality of life for longer, meaning that nursing home admission and expensive, intensive care required for more severe dementia, comes later down the line.
By delaying nursing home admission for 12 months, the modelling shows that an annual saving of £44,900 per patient could be made. Delay nursing home admission by six months and save £21,000. Make a £9,000 saving by delaying admission by three months. ***
Where does this £44,900 figure come from?
- Local authorities could save an estimated £38,000 per year for every patient for whom they can delay nursing home admission.
- Patients could save £10,100 over the course of a lifetime
- The NHS would spend an upfront cost of £3,300 for early diagnosis and treatment
This research is restricted to AcHE inhibitor drugs for people with Alzheimer’s disease but there are several symptomatic dementia treatments available. However, it is estimated less than 6% of dementia patients are using these dementia-specific and antipsychotic drugs. In short, we’re not doing nearly enough of what works and that must change if we are to prevent catastrophic system pressure and cost.****
More research is needed to fully understand the impact of the available treatments. What we do know is that they are most effective the earlier they are given. To achieve these savings, we need to diagnose people and diagnose them earlier.
A lack of early diagnosis is associated with increased costs through higher rates of admission to hospitals and residential care. A recently published paper from the Lancet Commission on Dementia noted that early diagnosis and intervention leads to potential economic benefits from preventing unnecessary admissions to hospitals.*****
We know that an earlier diagnosis is better for people with dementia and carers because it unlocks access to care and support and means they can plan for their future.
As Lord Darzi says, citing our evidence in his report, “there is an important challenge to improve the quality and quantity of care for people with dementia”. Quite.
Diagnosing the undiagnosed
The Government’s official policy is the NHS is broken, reflected most starkly in dementia by its failure to diagnose enough of those living with the disease. Here, again, there’s a choice on whether to continue with the status quo or take a different path. By 2040, the cost of dementia to the NHS alone is forecast to reach £13.5bn. Today, almost 1 million people with dementia access A&E every year and 1 in every 6 hospital beds is occupied by someone with dementia. People with dementia make 16.2million visits to the GP every year.
Over 250,000 people in England currently live with undiagnosed dementia. The new evidence shows that people who are undiagnosed are disproportionately drawing on healthcare resources. Those who are undiagnosed are three times more likely to visit A&E than people without the condition, accounting for 520,000 visits annually. Undiagnosed people with dementia use A&E more than people with mild, moderate and severe dementia.
The £42bn spent on dementia this year is equivalent to 23% of total NHS spend and 3.4% of total government spend. It is estimated one in three people born today will develop dementia during their lifetimes.
This is a challenge which must be faced and faced now.
And now we know in starker terms than ever before that the foundations for delivering better care for people, for easing pressure, for reducing cost – it all begins with improving diagnosis.
Diagnosis is also an opportunity to reduce the economic impact of dementia and repair our health and social care system.
Alzheimer’s Society is calling for:
- Bold, ambitious and achievable new diagnosis rate targets
- Improving the quality of diagnosis through dedicated funding
- Improvements to the recording, collation and analysis of dementia data including greater use of secure data environments (SDEs)
We want to work with you. Contact us: change@alzheimers.org.uk
Read The Economic Impact of Dementia.
Watch Anna Richardson: Love, Loss and Dementia on October 2nd at 10pm, Channel 4.
 References
References
* The Economic Impact of Dementia (2024)
** It is estimated around half of Alzheimer’s disease patients benefit from AChE inhibitor treatment.
*** Based on analysis of the English Prescribing Dataset, it is estimated less than 6% of all people with dementia were prescribed AChE inhibitors in 2023'
****Progression through stages of dementia (including Alzheimer’s disease) from mild cognitive impairment to severe dementia, is poorly documented. The literature isn’t conclusive, so the study has also modelled it delaying nursing home admission by 6 months and 3 months.
***** Livingston et al (2024). Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. P603.
